Crohn’s disease and ulcerative colitis are largely unfamiliar terms. Hundreds of thousands of Americans are affected by these conditions, however many people still don’t know how to identify the two, or understand how they relate and differ.
Crohn’s and colitis are both inflammatory bowel diseases (IBD), which result from an overactive immune response that treats the normal, healthy contents of the colon (such as good bacteria and food) as foreign invaders. When the immune system detects a foreign substance, it sends a sea of white blood cells to the site of this substance, which in turn causes inflammation. Victims of IBD struggle to experience healthy digestion that doesn’t involve their system getting unnecessarily attacked by an immune response.
The body’s reactions to these two diseases are often described similarly: loss of appetite, weight loss, urgent bowel movements, diarrhea, and fatigue. They are both long-term (chronic) conditions; individuals who are affected will likely have symptoms that come and go throughout their lives. The onset of symptoms tends to be inconsistent, and when there are time periods without symptoms the diseases are deemed to be in remission.
Stock Images of Crohn’s Disease and Ulcerative Colitis
Although Crohn’s and colitis have some similar traits, they are certainly not the same condition.
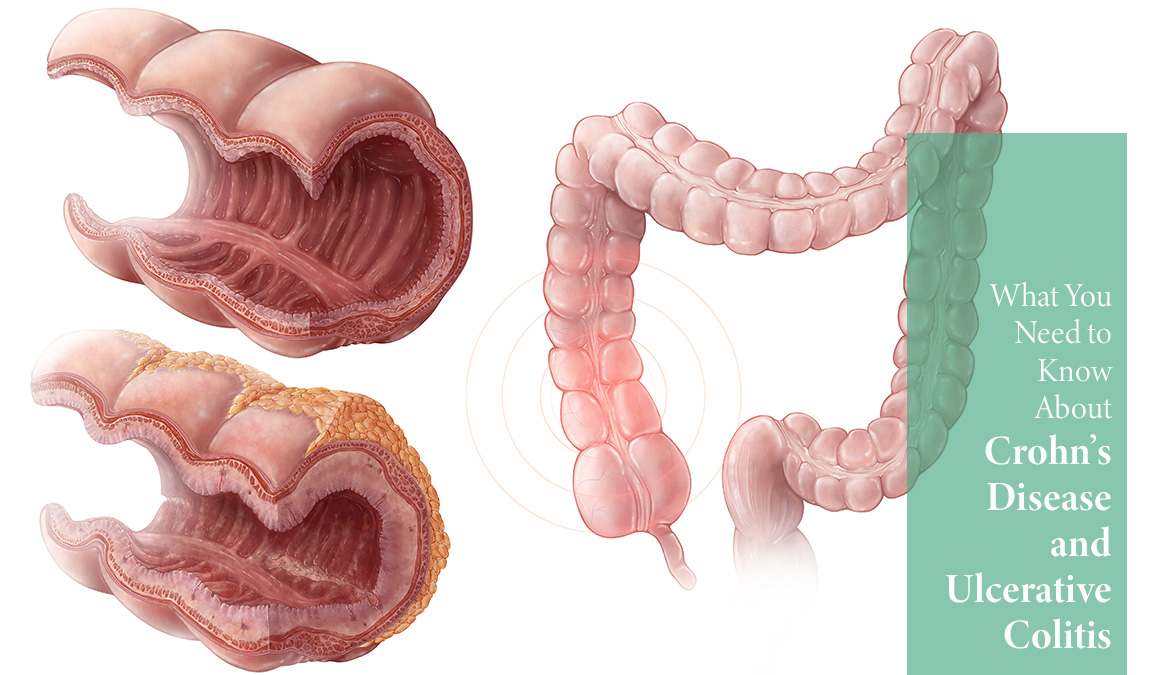
Ulcerative colitis causes inflammation that gives rise to ulcers in the inner lining of the colon (large intestine). The ulcers permit unwanted fluids such as mucous into the digestive system, which perpetuates irritation. It affects the colon exclusively, while Crohn’s disease can affect any part of the gastrointestinal (GI) tract, including the small intestine, large intestine, mouth, stomach, or anus.
While Crohn’s disease can affect many different parts of our anatomy, the most commonly affected site is the ileum, or the area that joins the end of the small intestine and the beginning of the colon. Unlike ulcerative colitis, Crohn’s can affect not only the inner lining of the intestine, but the entire intestinal wall. It is also known to ‘skip’ patches of the intestines, leaving some parts of the anatomy unaffected by the disease, and some parts inflamed and dilapidated. This pattern of damage throughout the bowels distinguishes Crohn’s from ulcerative colitis and other diseases.
The causes of both Crohn’s and colitis still remain somewhat of a mystery to researchers. Consistencies within studies that revolve around genetics have begun to pave the way towards some answers. Many people that have ulcerative colitis have a family member that is also affected; if someone in your family has Crohn’s your chances of developing the disease may be higher.
There have also been studies on environmental factors, finding Crohn’s disease more common in industrialized countries than in the developing world, and more common in urban areas rather than areas encompassed by farmland. Stress and high-fat diets are thought by some to be contributing factors as well, and may trigger an existing condition.
Even if you have family members that suffer from these diseases and are experiencing some of the common symptoms, it is important to be tested by a physician. Multiple tests, including physical exams and diagnostic scans, are often required for a proper diagnosis.
Although there is no cure for ulcerative colitis or Crohn’s disease, there are many different kinds of medicines available to keep symptoms at bay and remission intact. Researchers are continuing to study possible causes, however these conditions have thus far remained puzzling, even to experts.
crohnscolitisfoundation.org
niddk.nih.gov/health-information/digestive-diseases/crohns-disease
niddk.nih.gov/health-information/digestive-diseases/ulcerative-colitis